I have some great questions about Insulin Pumps today.
At this point, I will now take a moment and apologize because I have pumped for 12 years & have the benefits of being covered for insulin pump therapy throughout this time, I assume everyone knows what I know about them. I also assume, if they have the ability to, they would automatically want to be on one. That is very ignorant of me and I’m sorry. I started Diabetes Beyond Borders for this very reason, to educate and give as much information to empower you. Unfortunately I missed the mark on this one.
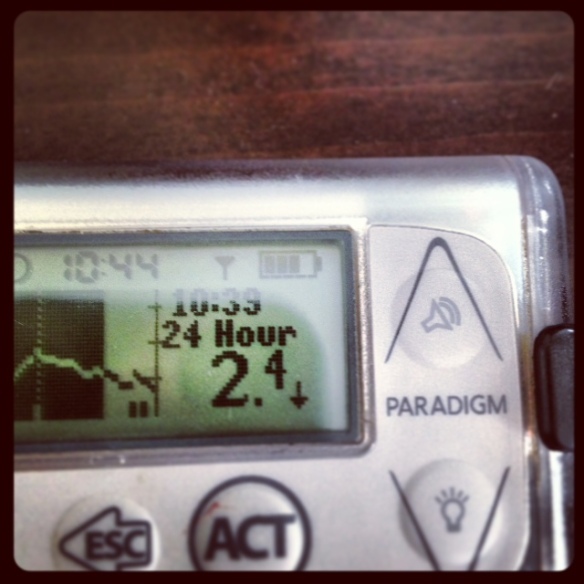
One more small disclaimer. I worked as a Territory Manager for Medtronic Inc. selling Paradigm Insulin Pumps. This Blog will not sell one pump over another. At this point I am now doing Insulin Pump starts & follow-up for Medtronic and Accu-Chek. As a Health Care Professional, peep living with Type 1 & Mom of a Type 1, my aim now is to give you an unbiased summary about Insulin Pump Therapy so that you can research more to see if pumping is right for you & which one best suits your lifestyle & needs if you decide to.
So…here we go….
SIZE: In general, all pumps are bigger then a pager but smaller than a cell phone. Many people have mistaken mine for a pager or cell. In the picture in my hand is one of the smaller ones. I don’t need a lot of insulin, so I use a smaller pump.
COLOURS: You want colour it, you got it. There is charcoal, clear (like mine), pink, green, purple… You can buy covers & skins to decorate it anyway you see fit. I like the clear one because I wear mine in my bra a lot…I don’t want it to be seen through my shirt. A lot of guys like charcoal because it looks more like a pager.
PARTS OF THE PUMP 101:
1. BUTTONS: Used to navigate the pump. About 5 buttons on the face/front of it, some pumps have ~1 or 2 on the side as well.
2. REMOTE: Some pumps have remotes that work also as the glucose meter. Not all have this.
3. CARTRIDGE: Fits in the pump which has Rapid Acting insulin such as NovoRapid, NovoLog, Humalog, Apidra (when on a pump you no longer take Long Acting insulin such as NPH, Levemir or Lantus). The cartridge is plastic.
4. TUBING: It is attached to the cartridge of insulin which comes in various lengths, as short as 18″ to as long as 43″ & a few lengths in between. The tubing is flexible & durable. There is a new ‘patch’ pump on the market that does not have tubing.
5. INFUSION SET: This is the teflon tube or needle that sits under your skin to deliver the Rapid Acting insulin. The tubing connects to the infusion set. It can be connected & disconnected as needed for showering, activity,or intimate moments. There are a variety of infusion sets to choose so that you have the right one for your lifestyle.
BASIC FUNCTIONS OF THE PUMP:
1. BASAL RATE: I call this the ‘base’ or ‘fasting’ delivery of insulin that your pancreas would be doing for you if you didn’t have diabetes. The Long Acting insulin you are taking tries to do this through 1 or 2 injections per day. On the pump, you can customize your basal rate to meet the different needs your body has throughout the day. You can make these changes on an hourly basis if needed. Most people only need 3 − 5 different basal rates during a 24 hour period. They do not change often after they have been established. BUT, the beauty is, you can change them and the time of day you need to. Basal rates are delivered in very small increments throughout the day, each pump delivers the rate based on its own calculation in which that company feels is best for their product but at the end of the day, the delivery is balanced & tiny enough it provides better balance when you are not eating. It is easier to skip a meal or get off schedule without suffering the consequences of a low blood sugar because of the features of a basal rate.
2. BOLUS: Essentially it is the Rapid Acting insulin you inject with. The beauty? The tube is already under your skin so you don’t have to inject. The other benefit is the pump does all the work to calculate your insulin dose. The increments that can be delivered on a pump can be as small as 0.025 units and as big as 35 units. I imagine now your routine on injections involves adding up your carbs, trying to decide how much extra to adjust for a high or low BG, taking a calculator or phone & crunching the numbers to find how much you will inject with your pen or syringe, which usually has to be rounded up or down to the nearest half or full unit of insulin. The built-in bolus calculator allows you to input your BG (usually remotely through the glucose meter), input your carbohydrates. The pump then shows you the breakdown of why it has decided you need a certain amount of insulin. It considers a correction for your sugar to bring it to target, whether that means adding extra to treat a high or subtracting some off to avoid a low. It also shows the carbs you chose & how much insulin you will get based on that. It also takes into consideration how much insulin you still have in your body. Having bad lows from unaccounted insulin still floating around in your body will be no more. The pump remembers.
3. BG READINGS: The pump stores your readings if you enter them into it, whether manually or through your remote meter.
4. CARBS: The pump keeps a history of the carbs you have eaten, when & how much insulin.
5. INCREMENTS: The increments on the basal rate & bolus can be as small or as large as needed. Some pumps vary, so make sure the one you choose fits your needs. Type 1 & Type 2 peeps do very well on pumps for this reason.
6. DELIVERY: The rate a pump delivers insulin varies from pump to pump. Be aware how comfortable you are with the rate it infuses into you.
7. SENSOR: There are only 2 companies that I am aware that offer Continuous Glucose Sensor technology; Medtronic & DexCom. I will post another Blog about this technology. It is far too complex to include it in this one. Suffice to say, having used the technology personally, I see the impact it has on diabetes management & glycemic control.
RESPONSIBILITIES AS A PUMPER:
1. BG TESTING: At least 4 times per day and more often as necessary.
2. INFUSION SET/CARTRIDGE CHANGE: Infusion sets need to be changed every 2 − 3 days, depending on the set you choose. Some companies are saying to change the cartridge & tubing every 3 days, others support 6 is the way to go.
3. DIABETES KETO-ACIDOSIS PROTOCOL: With only having Rapid Acting insulin in your body, it is only in a matter of hours that you will ‘run out’ of insulin in your body if something doesn’t work with your pump. It is easy to trouble shoot & correction can be quick. The trick is to be acutely aware when you test high & adhere strictly to protocol to treat the high sugar. It is rare it can happen but when it does it is SO important to follow the few simple steps it takes to correct it.
WHERE TO WEAR THE PUMP
There is an assortment of clips, pouches & belts that are available from pump companies & online stores. This allows you to decide whether you want it under your pants on your calf, under your skirt around your thigh, clipped on your belt or around your waist, in your bra, around your arm. Creativity, convenience & comfort are key. I know many with careers from police officers, construction workers, nurses, teachers etc that find living with their insulin pump provides better quality of life for them. It is trial and error of where to place it at first, but once you get your groove, it’s a no-brainer. You’ll forget it’s there.
PROS OF A PUMP:
1. Less low sugars
2. Less variability
3. More flexibility with lifestyle & scheduling
4. Less needles
5. Ability to pro actively prevent low & high sugars with activities, exercise, work etc.
6. Less calculating
CONS OF A PUMP:
1. Have something attached to you 24-7
2. Remembering to change the infusion site, tubing & cartridge on time. (I developed a system to help me remember, some pumps have a reminder in it)
WHAT TO CONSIDER WHEN BUYING A PUMP
1. Ease of Use
2. Technology available that suits your needs
3. Software available to download the results to manage your diabetes
4. Cartridge size (they come in 1.8 mL, 3.0 mL, 3.15 mL)
5. Insurance Coverage
6. Long term costs
7. Pump Company Customer Support
8. Ease of ordering supplies
9. Features within the pump that meet your needs
10. Basal & Bolus delivery increments that meet your insulin needs
11. Infusion set choice (one pump company’s sets are proprietary so you will need to order their supplies only, make sure they have what you want)
12. Some companies require you replace your battery cap & cartridge cap every 3 months. It will be at a cost to you. Make sure to ask about this.
13. Some pumps are waterproof & some are water tight. I have always put it this way…I wouldn’t swim with my cell so why would I swim with my $7,000 pump. Especially in a lake…if it goes to the bottom of the lake there is no getting it back.
I liken deciding to pump & choosing one to buying a car. It’s a long-term, expensive decision you will live with for 4 − 5 years. Shop wisely & make sure to ask a lot of questions. If you have the option to trial one using saline in the cartridge before buying, I urge you to do it.
Always keep in mind:
1. All companies give a 4 year warranty.
2. You have 90 days after you order your pump to return it. If you decide it’s not the right one & you want a different one OR if pumping just isn’t for you. There is no cost to you to return it.
3. Please, please make sure to add your pump to your house insurance policy. If your pump is stolen (which I know people it has happened to!), you want the reassurance you can get it replaced.
You can email me at tracy@diabetesbeyondborders.com with any questions. I am here for you.
 With the exception of the time we dated in high school, my husband Steve is diagnosed with Type 1 spousal diabetes for just under four years.
With the exception of the time we dated in high school, my husband Steve is diagnosed with Type 1 spousal diabetes for just under four years.